Medical students have long faced a fundamental challenge: learning three-dimensional anatomy from two-dimensional textbooks. The disconnect between flat diagrams and actual human bodies creates gaps that only become apparent in clinical settings.
VR medical training closes that gap by placing learners inside immersive, interactive environments where they can explore anatomy, practice procedures, and develop clinical skills without risk to patients. This guide covers how the technology works, why institutions are adopting it, and what it takes to implement VR in healthcare education programs.
What is VR medical training
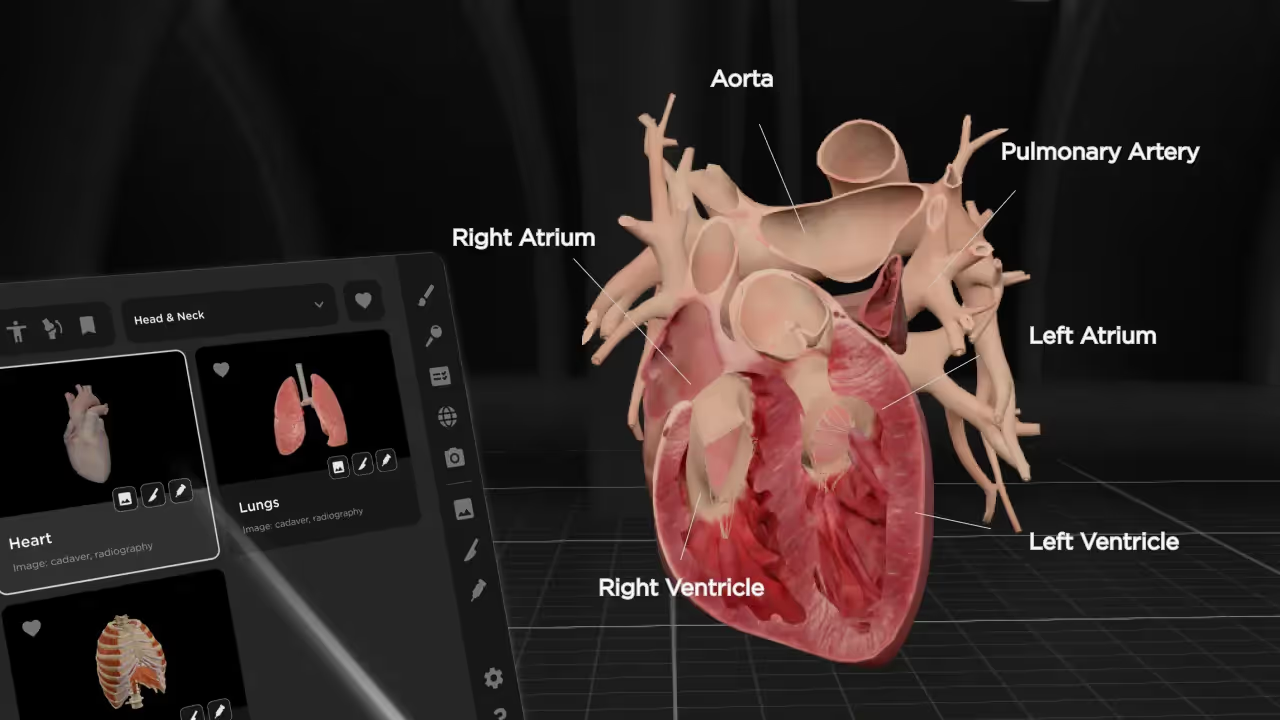
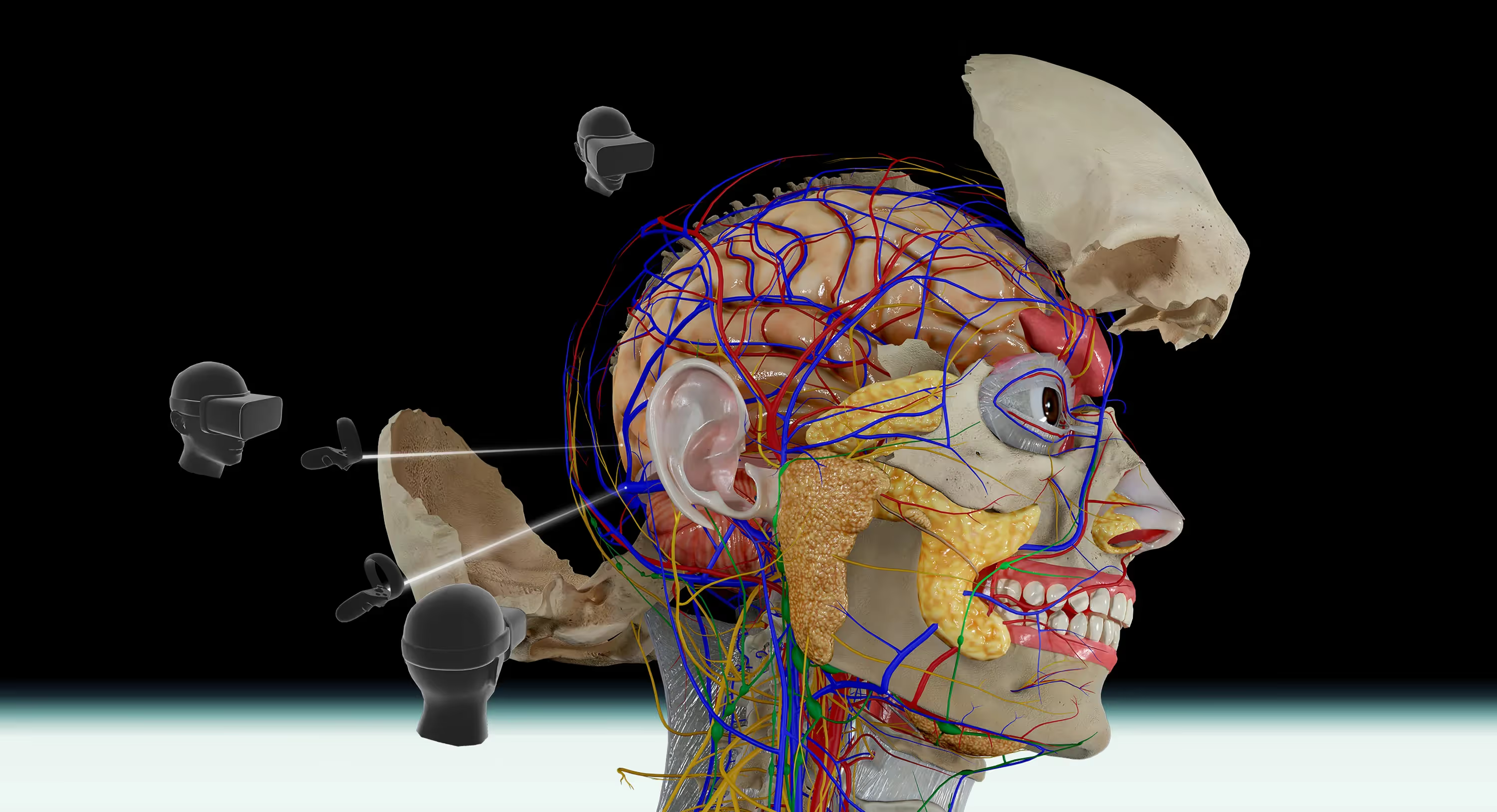
VR medical training uses immersive, computer-generated environments to teach clinical skills, anatomy, and patient care. Learners wear headsets to interact with three-dimensional simulations of the human body, medical procedures, and patient scenarios. Instead of watching a video or flipping through a textbook, you're placed inside the learning experience itself.
The term covers a wide range of applications. Some platforms focus on anatomy visualization, letting you explore body structures layer by layer. Others simulate surgical procedures or emergency room scenarios. What ties them together is the immersive quality—you're not just observing, you're doing.
Modern VR medical training runs on devices like Meta Quest and HTC Vive headsets, which have become increasingly affordable and accessible. This means medical schools, nursing programs, and healthcare institutions can adopt the technology without building expensive dedicated facilities.
Why VR is transforming healthcare education
So why are healthcare institutions adopting VR at such a rapid pace? According to the Association of American Medical Colleges, 68% of U.S. medical schools have already adopted VR or AR into their curriculum as of 2024. The short answer: it solves problems that traditional methods have struggled with for decades.
Improved spatial understanding of anatomy
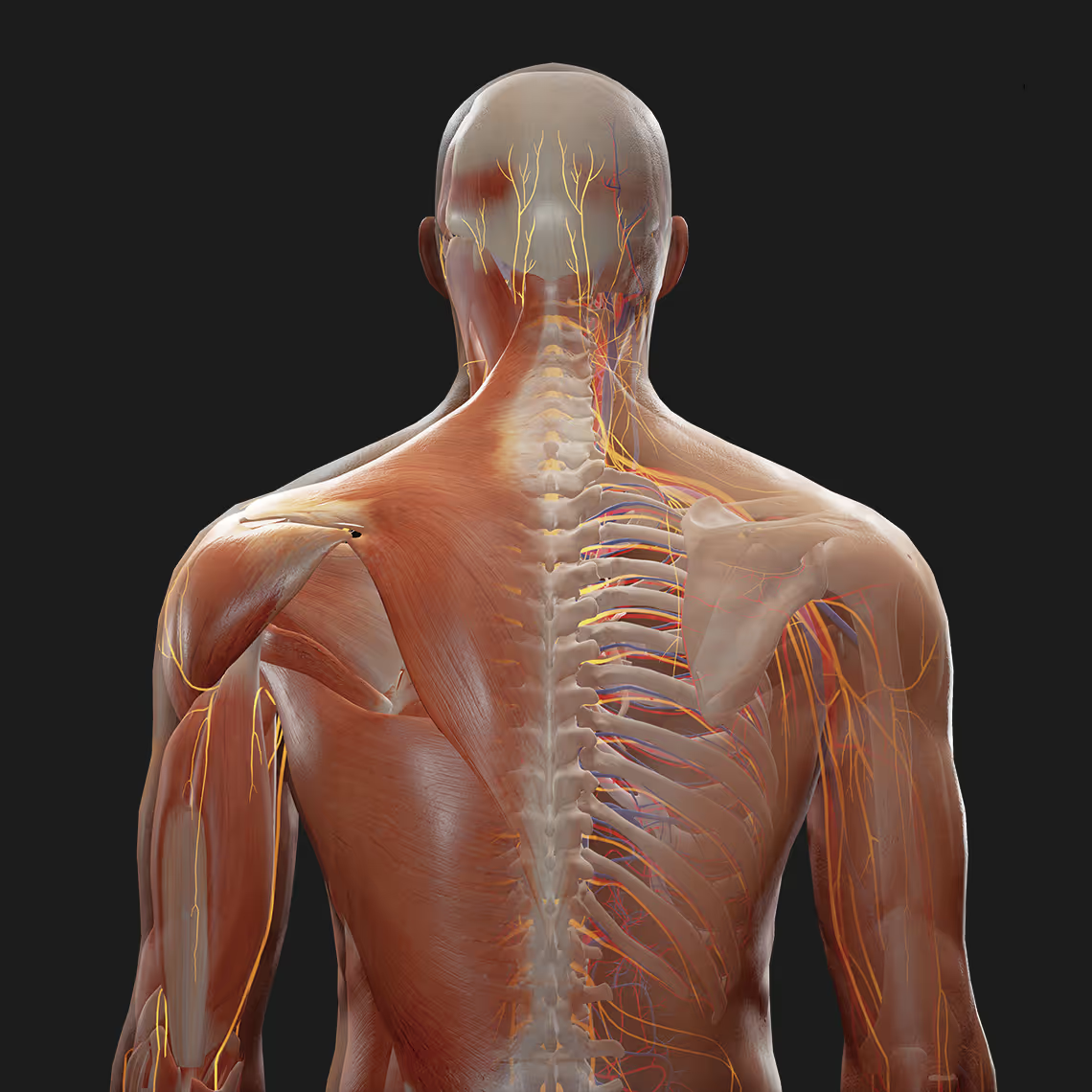
The human body is three-dimensional, yet most students learn it from flat images in textbooks. This creates a gap between what students see on paper and what they encounter in clinical settings.
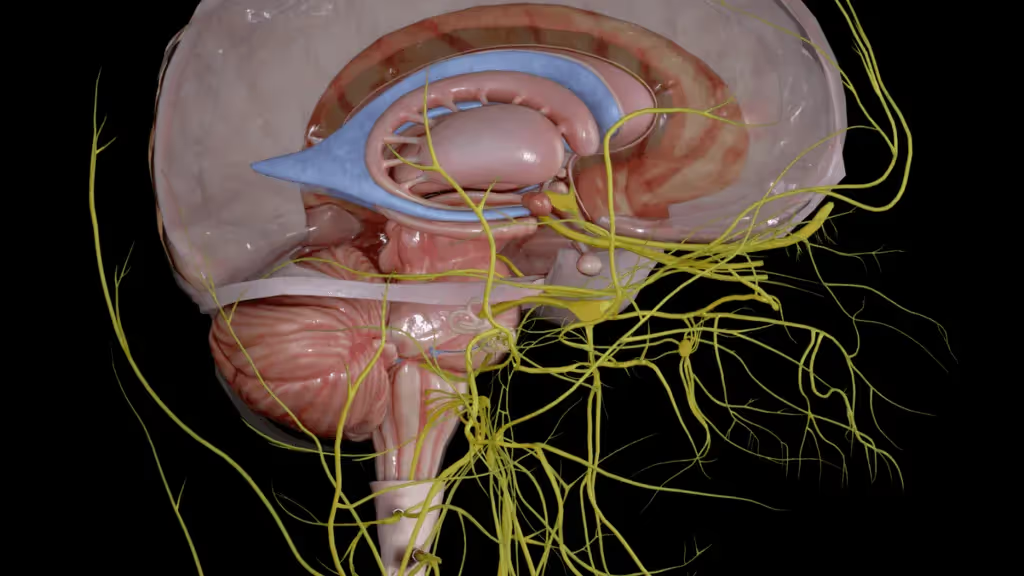
VR closes that gap. With platforms like BodyMap, you can rotate anatomical structures, isolate specific systems, and explore how organs, vessels, nerves, and muscles connect in real space. It's similar to the difference between studying a city on a paper map versus actually walking through its streets.
This spatial awareness matters because clinicians navigate actual bodies during examinations and procedures. Knowing that a nerve runs behind a particular muscle, or that an artery sits just beneath a specific bone, can make the difference between a successful procedure and a complication.
Better knowledge retention and recall
Here's something interesting: immersive learning engages the brain differently than passive study.
Neuroscience research has shown increased activity in the hippocampus—the brain region responsible for memory formation—when learners engage with virtual environments compared to static images. The brain treats VR experiences more like real experiences, which helps information stick.
For medical students facing enormous volumes of material, this retention advantage is significant. What you learn in VR tends to stay with you longer than what you memorize from a lecture.
Safe practice without patient risk
One of VR's most valuable qualities is the freedom to make mistakes.
In a virtual environment, you can attempt a procedure incorrectly, see what happens, and try again. No patient is harmed. No instructor has to intervene. This psychological safety creates space for genuine learning through trial and error.
Traditional clinical training, by contrast, requires careful supervision and limits how much hands-on practice students can get before working with real patients.
Scalable training for large student cohorts
Cadaver labs are expensive, limited in capacity, and constrained by preservation timelines. Physical simulation mannequins require storage, maintenance, and scheduled access. These resources don't scale easily.
VR removes those bottlenecks. A single virtual body can serve unlimited learners simultaneously, from anywhere with a headset. For institutions with growing enrollment or limited physical resources, this scalability changes what's possible.
Higher student engagement in learning
Let's be honest! Anatomy lectures can be dry. VR introduces interactivity that increases motivation and active participation.
When you can reach out and manipulate a beating heart or trace a nerve pathway with your own hands, you're engaged in a way that passive listening doesn't achieve. Studies show over 90% of students believe VR enhances their anatomy learning experience compared to traditional models. Engaged learners tend to retain more and develop deeper understanding of the material.
Key use cases for virtual reality medical training
VR in healthcare education spans multiple applications, each addressing different learning objectives.
Anatomy and physiology visualization
Medical students use VR to study body structures layer by layer, gaining spatial awareness that's difficult to achieve through other methods.
- Dissection simulation: Virtually remove layers to view underlying structures without the limitations of a single cadaver
- System isolation: View only the cardiovascular, nervous, or skeletal system to focus your study
- Spatial orientation: Trace how structures connect and relate in three-dimensional space
With BodyMap, for example, you can select a nerve, trace it back to its origin, and see its pathway through surrounding tissues. This kind of exploration is nearly impossible with textbook diagrams alone.
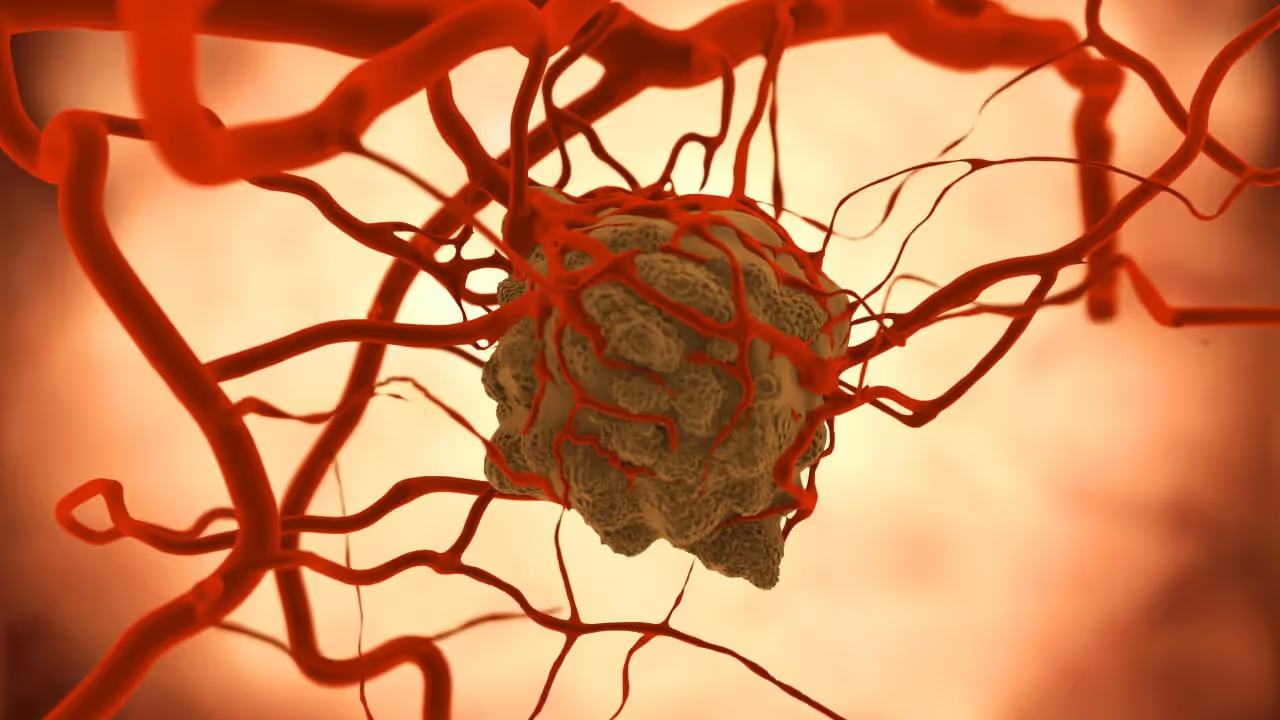
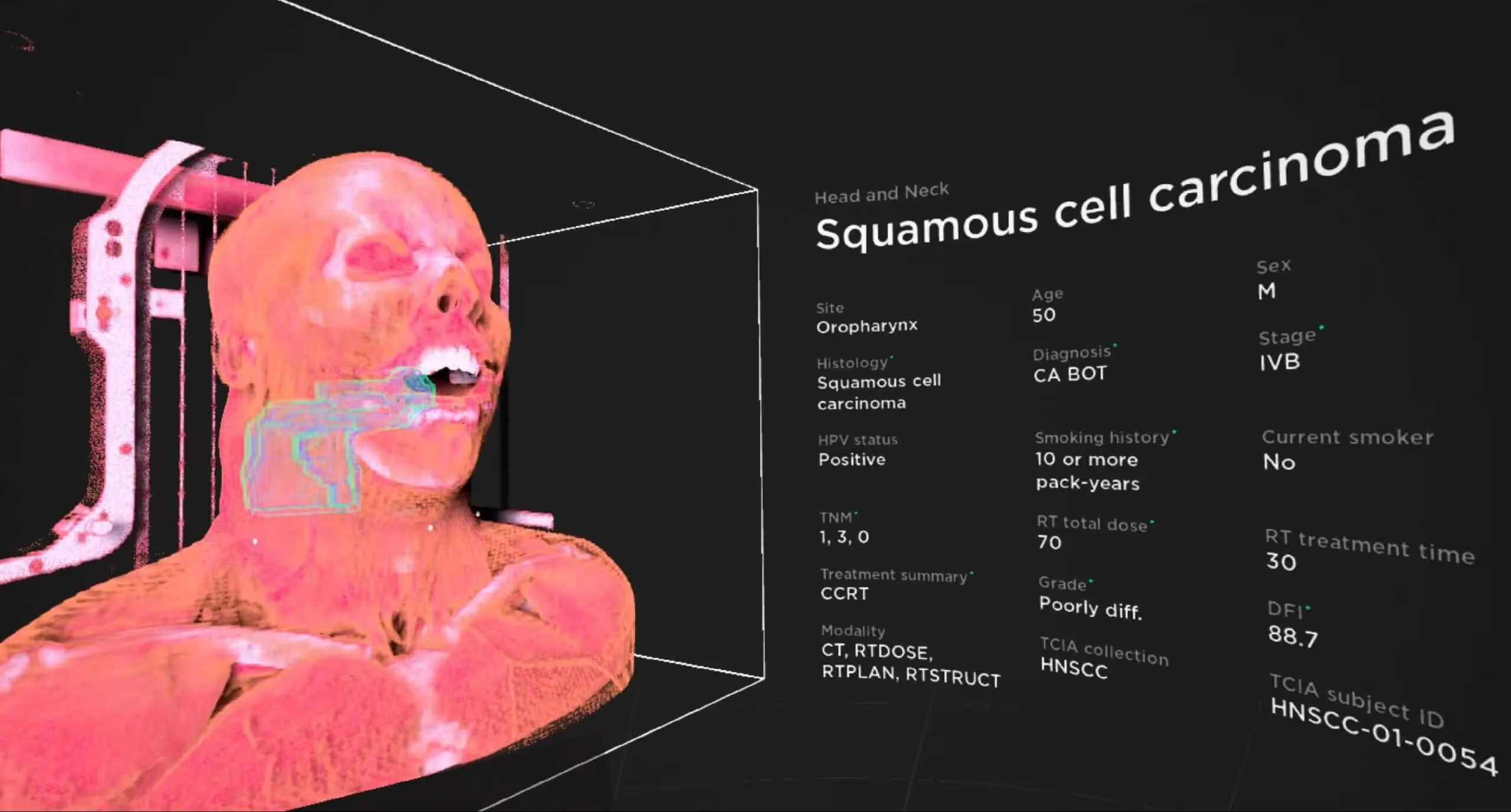
Surgical skills and procedure practice
VR surgical simulators let trainees practice incisions, suturing, and instrument handling before entering the operating room. Many platforms provide haptic feedback and performance metrics, allowing learners to refine technique through repetition.
Emergency medicine and critical care simulation
High-pressure scenarios like cardiac arrest or trauma response require quick thinking and practiced responses. VR recreates these situations safely, allowing repeated practice until responses become automatic.
Nursing clinical competency training
Nursing students use VR to practice patient assessments, IV insertion, medication administration, and other clinical skills, while acupuncture students practice point location and needle insertion techniques. The technology provides a bridge between classroom learning and actual patient care.
Patient communication and soft skills development
Not all medical training involves technical procedures. VR scenarios with virtual patients help learners practice bedside manner, delivering difficult news, and conducting clinical interviews.
How VR compares to traditional medical training methods
To understand where VR fits, it helps to compare it directly with established approaches.
VR doesn't necessarily replace traditional methods entirely. Many programs find the greatest value in using VR to supplement cadaver labs and clinical rotations, extending practice opportunities beyond what physical resources allow.
Research supporting virtual reality in medical education
The evidence base for VR in medical training continues to grow, with research spanning neuroscience, educational outcomes, and long-term retention.
Neuroscience of immersive learning
Brain imaging studies consistently show that immersive environments activate memory-related regions more strongly than passive learning formats. This neurological engagement translates to better encoding and recall of complex information.
Medical school performance outcomes
Medical school partners using VR anatomy platforms report that students demonstrate improved confidence and express strong preference for immersive learning. While VR is relatively new in medical curricula, early outcome data is encouraging.
Long-term retention improvements
Research indicates that VR-learned information resists the forgetting curve more effectively than lecture-based learning. For medical students facing board exams months after initial coursework, this retention advantage matters.
How much does virtual reality medical training cost
Cost is often the first question institutions ask when evaluating VR adoption. The answer depends on several factors.
Software licensing and subscriptions
VR training platforms typically charge per-seat licenses or institutional subscriptions. Pricing varies based on content library size, features, and user volume. Some platforms offer tiered pricing that scales with institutional size.
VR hardware and equipment
Standalone headsets like Meta Quest have made VR more affordable than ever, no expensive gaming PCs required. However, institutions still need to budget for multiple devices, protective cases, and hygiene considerations for shared equipment.
Implementation and faculty training
Beyond hardware and software, institutions should budget for instructor onboarding, IT support, and curriculum integration time. Faculty comfort with the technology directly impacts student adoption and learning outcomes.
How to implement VR training in healthcare education
Adopting VR requires thoughtful planning. Here's a practical sequence for institutions considering implementation.
1. Define learning objectives and training needs
Start by identifying which courses or competencies will benefit most from VR. Anatomy, procedural skills, and emergency response are common starting points where VR's strengths align well with learning challenges.
2. Evaluate and select a VR platform
Research platforms based on content relevance, device compatibility, and evidence of learning outcomes. Consider whether anatomy-focused tools or procedure simulators best fit your curriculum.
3. Acquire VR hardware and set up infrastructure
Select headsets compatible with your chosen software. Ensure adequate WiFi bandwidth, charging stations, and secure storage for equipment.
4. Train instructors on VR tools and best practices
Provide faculty with hands-on training before student rollout. Address common technical issues and discuss pedagogical approaches for integrating VR into existing lesson plans.
5. Integrate VR into existing curriculum
Map VR modules to specific learning objectives and assessment criteria. Position VR as a supplement that enhances rather than entirely replaces traditional methods.
Challenges of VR in medical and healthcare training
Adopting any new technology comes with obstacles worth acknowledging.
Faculty technology adoption
Some instructors may feel uncertain about new technology. Adequate training and clear demonstration of learning outcome improvements help build faculty confidence.
Upfront investment requirements
Initial hardware and software costs can be significant, though long-term savings often offset ongoing cadaver and lab expenses. Institutions should view VR as a multi-year investment.
Motion sickness and user comfort issues
Some users experience VR-induced discomfort, particularly during extended sessions. Modern headsets have improved significantly, and shorter session lengths help mitigate this issue.
Curriculum and accreditation alignment
Institutions need to ensure VR training meets accreditation standards and integrates with existing assessment frameworks. This may require documentation and communication with accrediting bodies.
The future of virtual reality and medicine
VR in medical training continues to evolve rapidly, with the market projected to grow from USD 7.61 billion to USD 87.42 billion by 2032.
Mixed reality—which blends virtual elements with the physical world—is emerging as a complementary technology. Imagine practicing a procedure on a physical mannequin while seeing virtual anatomical overlays through your headset.
AI-powered adaptive learning is another frontier, where VR platforms adjust difficulty and content based on individual learner performance. Multiplayer collaborative training allows students and instructors to share virtual spaces regardless of physical location.
Start your VR anatomy training journey
MAI's BodyMap platform offers an accessible entry point for medical and health sciences students, faculty, and institutions seeking immersive anatomy education. The platform runs on popular VR headsets including Meta Quest and HTC Vive devices, with detailed 3D models designed for learning spatial relationships between body structures.
Start a free trial of the BodyMap anatomy platform
FAQs about VR medical training
What hardware is required for virtual reality medical simulation?
Most VR medical training platforms support standalone headsets like Meta Quest or PC-connected devices like HTC Vive. Check software compatibility requirements before purchasing equipment, as some platforms work across multiple device types while others have specific requirements.
Can VR anatomy training replace cadaver dissection in medical school?
VR serves as a powerful supplement that provides unlimited, repeatable practice opportunities. Many programs use it alongside rather than as a complete replacement for cadaver labs, combining the strengths of both approaches.
How quickly do medical students adapt to VR learning environments?
Most students become comfortable navigating VR anatomy platforms within one or two sessions. Those familiar with gaming or other immersive technologies often adapt even faster.
Is VR medical training recognized by healthcare accreditation bodies?
Accreditation standards vary by region and specialty. Institutions should verify that VR modules align with their specific credentialing requirements and document how VR training maps to required competencies.
What is the difference between VR and augmented reality medical training?
VR fully immerses users in a computer-generated environment, blocking out the physical world entirely. Augmented reality overlays digital elements onto the real world, allowing learners to see both simultaneously—useful for applications like surgical navigation or anatomy overlay on physical models.
Begin your VR anatomy journey today, sign up for a 7-day free trial.
Curriculum Integration Guides
Learn how to navigate the 3D model and utilize the tools to master human anatomy—all in one place.

.avif)


.avif)


.avif)