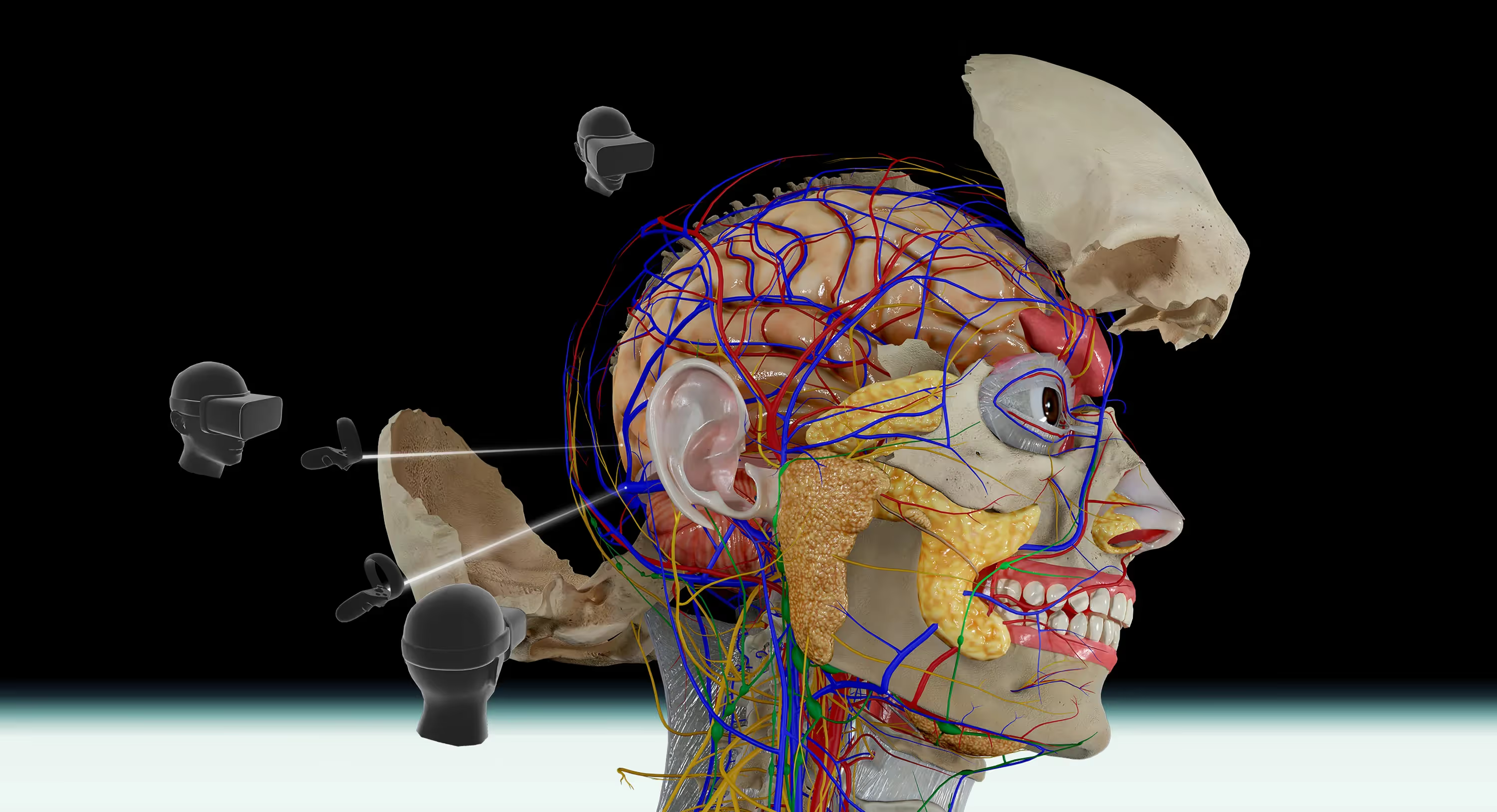
Medical students have learned anatomy the same way for over a century: standing around a cadaver in a cold lab, sharing scalpel time with seven classmates. Now VR headsets are challenging that tradition—and the research suggests they might teach anatomy just as well.
This guide breaks down what the studies actually show, where each approach excels, and how to decide whether virtual anatomy belongs in your curriculum.
Why medical schools are comparing VR and cadaver labs
Studies comparing VR anatomy tools to traditional cadaver dissection have found that students achieve similar test scores and learning outcomes with both methods. A peer-reviewed study in Anatomical Sciences Education showed that students using a VR skull model performed just as well on assessments as those studying with physical cadaveric skulls.
So what's driving this comparison in the first place?
Medical schools are facing a practical problem. Cadaver shortages affect institutions worldwide, procurement costs keep climbing, and class sizes are growing faster than lab capacity. At the same time, VR technology has matured to the point where it can deliver detailed, interactive 3D anatomy experiences.
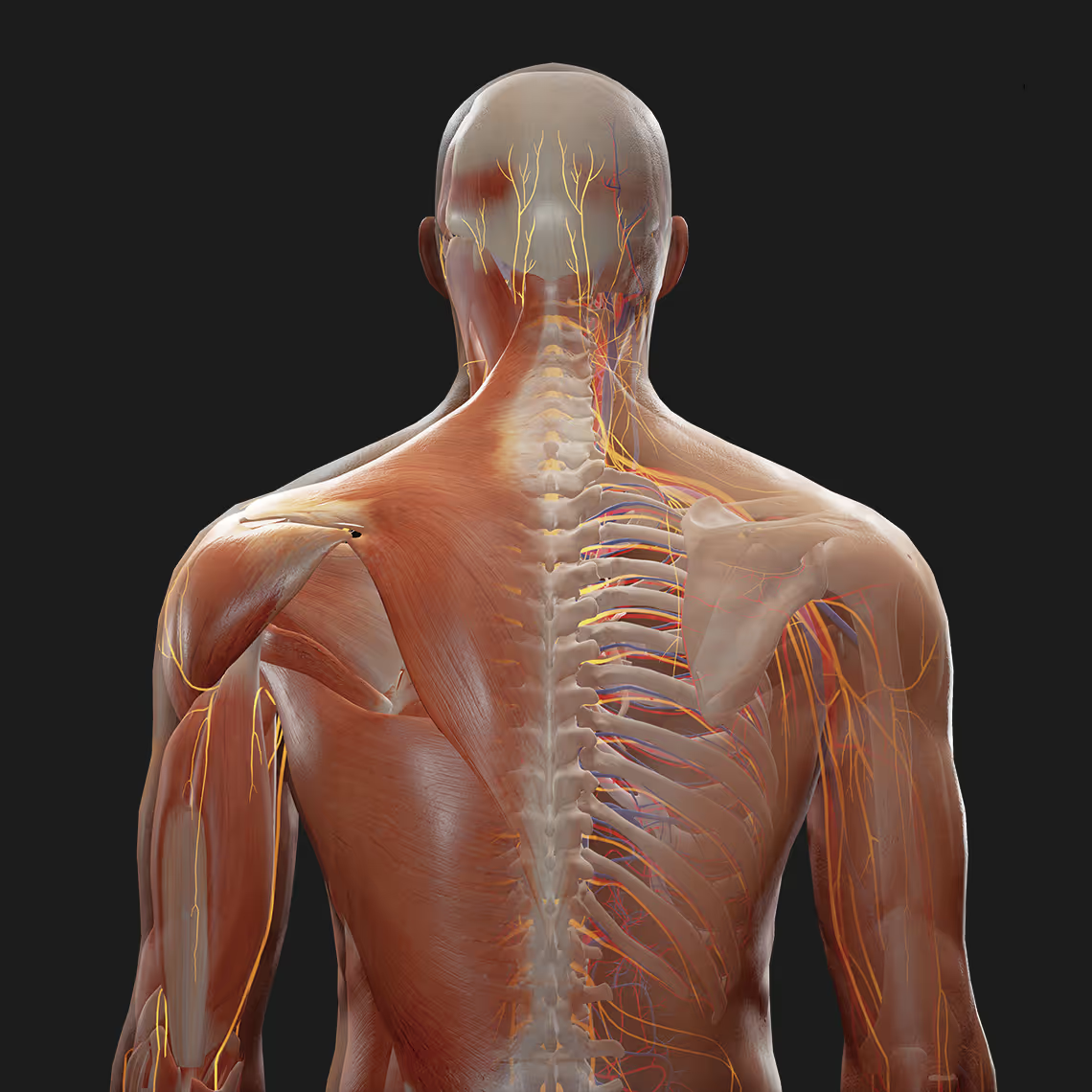
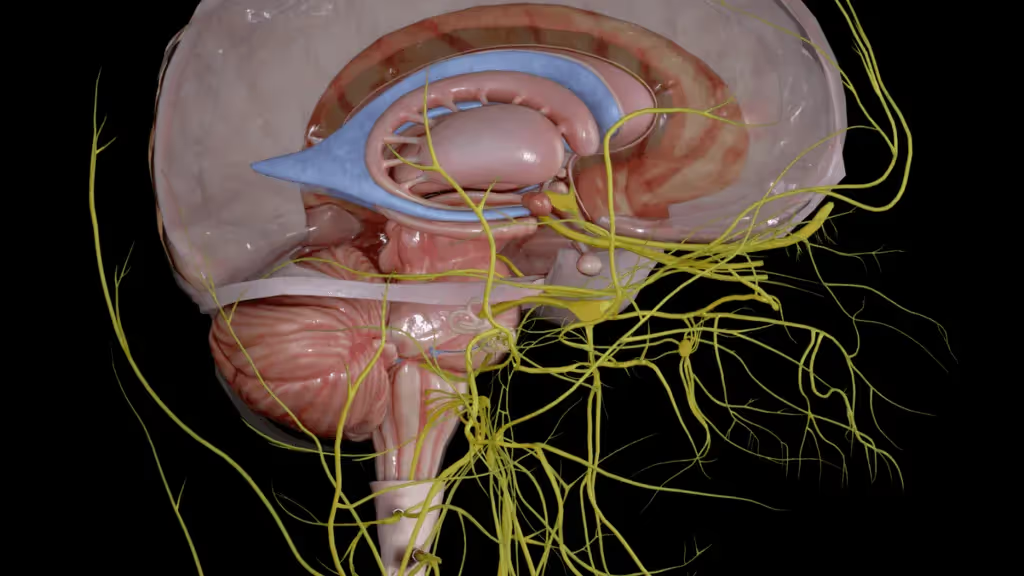
A "virtual cadaver" is a digital 3D model of the human body that students can explore, dissect layer by layer, and manipulate in a virtual anatomy platform.
The question educators are asking isn't whether VR is interesting. It's whether immersive technology can teach anatomy as effectively as the cadaver labs that have trained doctors for centuries.
What research says about VR vs cadaver effectiveness
Several peer-reviewed studies have now put VR anatomy training head-to-head against cadaver-based instruction. The results are consistent: students learning through VR achieve comparable knowledge gains, with VR showing significant improvement in knowledge scores compared to other methods.
Research from PrecisionOS found no significant difference in anatomy knowledge between students who trained with VR and those who used cadavers. The VR skull study mentioned earlier reached similar conclusions—equivalent performance on both identification tasks and spatial reasoning questions.
Here's what the research points to:
- Comparable test scores: Students using VR perform at the same level as cadaver-trained students on anatomy assessments
- Spatial reasoning: Immersive 3D environments help learners grasp how structures relate to one another in space
- Confidence levels: Students report feeling prepared for clinical applications after VR training
One reason VR seems to work so well comes down to how the brain processes immersive experiences. The hippocampus—the region responsible for forming memories—shows increased activity during virtual environment engagement compared to viewing static images. Active exploration creates stronger memory traces than passive reading or listening.
Benefits of VR anatomy education
Unlimited access and repeatability
With VR, a student can study at 2 AM before an exam or revisit a tricky structure dozens of times. There's no lab schedule to work around.
Physical cadavers can only be dissected once. Once you cut through a nerve, it's gone. Virtual anatomy lets students make mistakes, reset, and try again—a process that speeds up learning without permanent consequences.
Enhanced spatial understanding of 3D anatomy
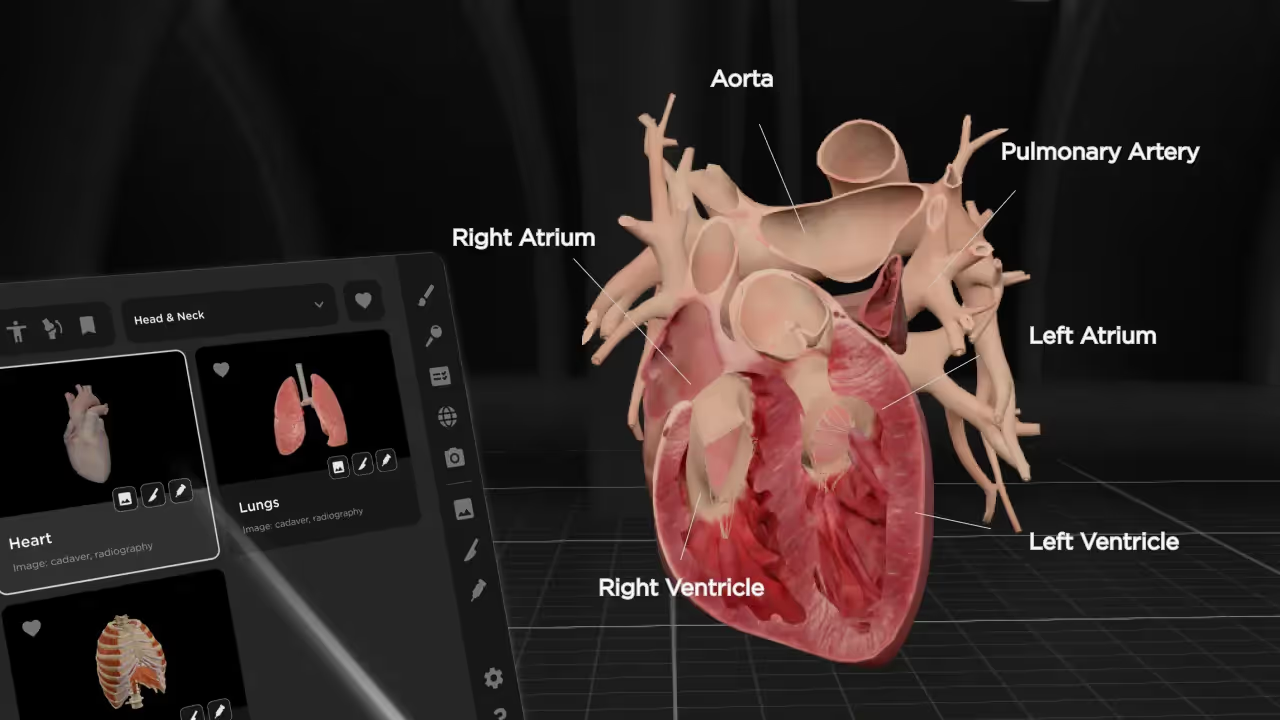
Textbooks flatten the body into two dimensions. Even excellent illustrations struggle to show how the brachial plexus weaves through the shoulder or how the heart sits in relation to the lungs and diaphragm.
VR changes this completely. Students can rotate structures, zoom into fine detail, and peel away layers to see what lies beneath, developing crucial spatial understanding.
With platforms like BodyMap, learners can trace a nerve from its origin all the way to its endpoint, building the kind of spatial intuition that's hard to develop from pages alone.
Stronger knowledge retention
People forget quickly. Traditional learning methods often result in significant information loss within days.
VR appears to counter this pattern. The immersive, active nature of virtual learning engages the brain differently than reading or lectures. Students aren't just receiving information—they're exploring, manipulating, and discovering it themselves.
Scalability for large student populations
A single cadaver might serve a group of eight students, with each person getting limited hands-on time. A VR platform can serve an entire class at once, with every student getting full access to every structure.
This matters as medical school enrollment grows—up 28.1% since 2013-2014. Institutions don't have to choose between educational quality and accommodating more students.
Ethical and logistical simplicity
Cadaver programs require donor consent processes, preservation facilities, biohazard protocols, and proper disposal procedures. Some students also experience significant emotional difficulty when first working with human remains.
VR removes these barriers. No formaldehyde, no cold storage facilities, no complex ethical considerations around body donation programs.
Benefits of cadaver-based anatomy training
Hands-on tactile experience
You can't feel tissue resistance through a VR headset. The sensation of separating muscle from fascia, the difference between an artery and a vein under your fingers—these tactile experiences remain unique to physical dissection.
For students heading toward surgical specialties, this hands-on practice builds manual dexterity that virtual environments can't yet replicate.
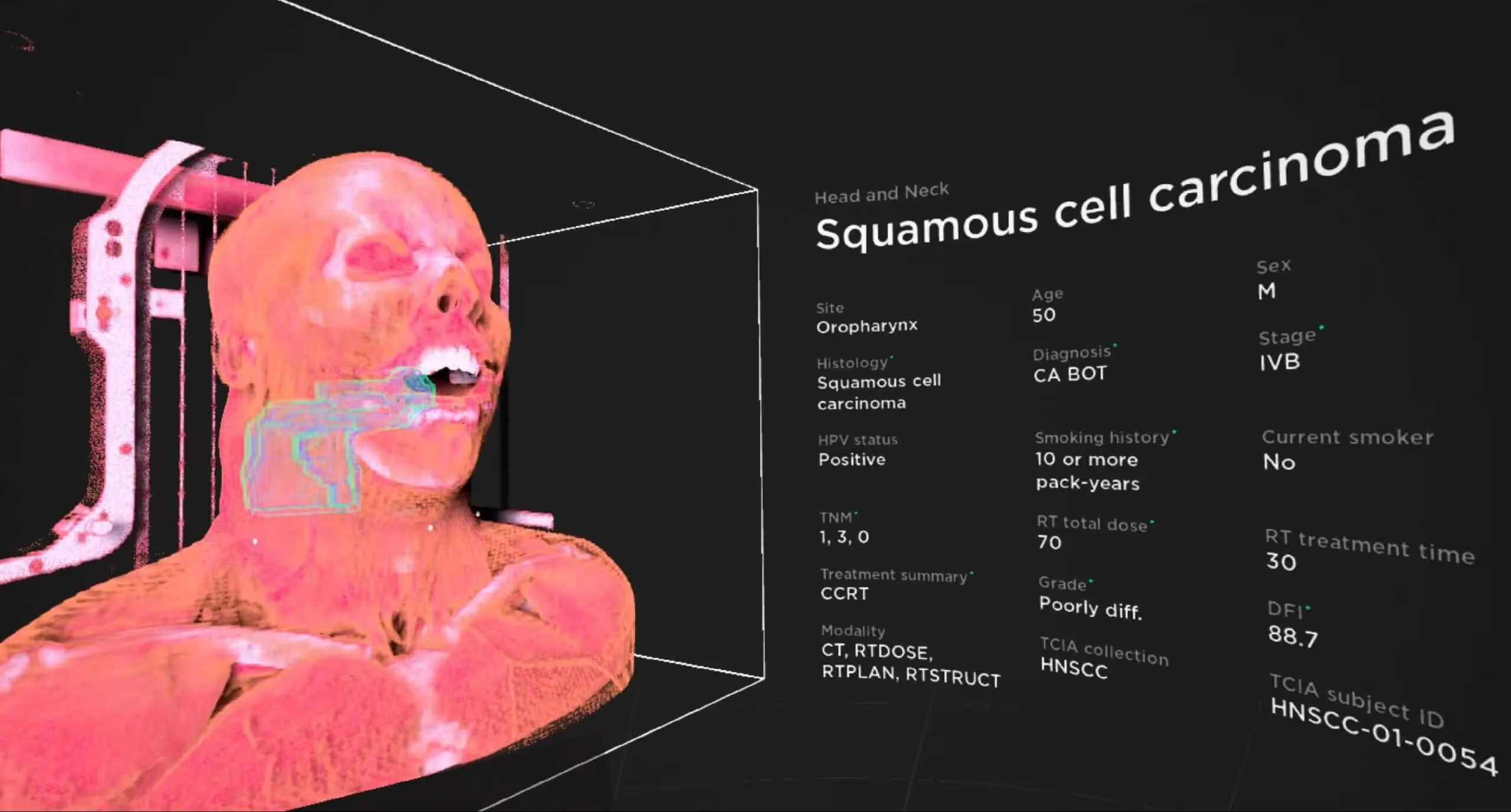
Exposure to real anatomical variation
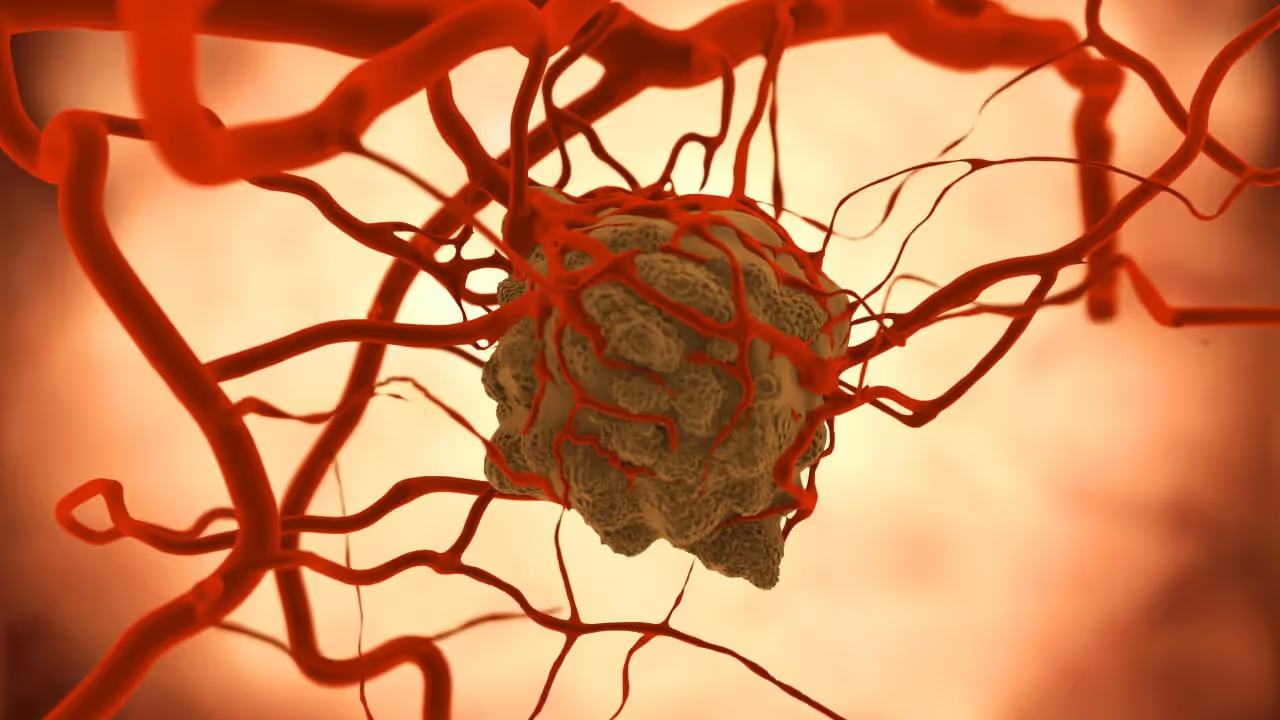
Every human body is different. Cadavers show natural variations in how vessels branch, where organs sit, and what pathological changes look like.
Standardized virtual models typically represent "textbook" anatomy. Encountering a patient with an unusual anatomical variant feels less surprising when you've already seen similar variations in the lab.
Emotional and professional preparation
Working with human remains teaches something beyond anatomy. It cultivates respect for the body, introduces students to death in a controlled setting, and contributes to professional identity formation.
Many educators argue this emotional preparation matters for future clinicians who will navigate difficult conversations with patients and families.
Limitations of virtual reality anatomy tools
Absence of tactile feedback
Current VR technology excels at visual and spatial learning but falls short on touch. Haptic feedback systems are improving, yet they don't replicate the nuanced sensation of handling real tissue.
This gap matters most for procedural training where feel is essential—knowing how much pressure to apply, recognizing tissue planes by touch.
Potential motion discomfort
Some users experience simulator sickness during extended VR sessions. Symptoms can include nausea, dizziness, or eye strain. While most people adapt over time, this remains a barrier for a subset of learners.
Technology and infrastructure requirements
VR requires headsets, compatible software, adequate physical space, and technical support. Faculty benefit from training and instructor resources before introducing VR tools to students.
The initial learning curve can feel steep, though platforms designed specifically for education prioritize ease of use for both instructors and students.
Limitations of traditional cadaver programs
High procurement and maintenance costs
Donor programs, preservation chemicals, specialized storage facilities, and disposal services add up. Many institutions spend substantial portions of their anatomy education budgets on maintaining cadaver labs.
Limited access and availability
Cadaver shortages are real, particularly in certain regions. Students often share specimens in groups, which reduces individual hands-on time significantly.
Lab hours are also limited. You can't study a cadaver at midnight the way you can open a VR application on your own schedule.
Preservation effects on tissue quality
Embalming changes tissue properties. Preserved specimens lose their natural color, texture, and pliability. What students see in the lab doesn't fully represent what they'll encounter in living patients during clinical rotations.
How students and faculty perceive VR vs cadaver learning
Student feedback on VR anatomy tools has been consistently positive. Surveys show over 90% of students indicated VR would enhance their anatomy learning experience, with high engagement levels and reduced anxiety compared to cadaver labs.
- Engagement: Students rate VR experiences as more engaging and less intimidating than traditional dissection
- Teaching flexibility: Instructors appreciate being able to demonstrate structures in real-time and guide students through complex regions
- Preference patterns: Many programs find students value having both options available
"The continuity of how BodyMap can pull up different structures and trace them back when you start with something as simple as one is astounding," shared Katie, a medical student from The University of Toledo.
She pointed out that a big part of her curriculum involves not only knowing anatomical structures but also understanding how they relate to one another. With BodyMap, she could look at the supraorbital foramen on the skull, then select a nerve and track it back to the trigeminal ganglia—something difficult to do cleanly in a physical dissection.
Should VR supplement or replace cadaver labs
The honest answer depends on your program's goals.
For foundational anatomy education—learning to identify structures and understand spatial relationships—VR can serve as a primary teaching tool. The research supports equivalent learning outcomes, and the practical advantages are substantial.
For surgical training programs where tactile skills matter most, cadaver experience likely remains valuable. However, even these programs can use VR to prepare students before they enter the lab, making physical dissection time more efficient.
The emerging consensus favors hybrid models—using VR to build foundational knowledge and spatial understanding, then supplementing with targeted cadaver experiences where tactile learning matters most.
How to implement VR anatomy training at your institution
Hardware and software requirements
Most VR anatomy platforms support popular headsets including Meta Quest and HTC Vive devices. BodyMap works across multiple hardware options, giving institutions flexibility in purchasing decisions.
You'll want adequate physical space for students to move safely while wearing headsets, plus reliable WiFi for any cloud-based features.
Faculty training and curriculum integration
The technology works best when faculty feel comfortable using it. Hands-on training sessions before introducing VR to students help instructors integrate the tools naturally into their teaching.
VR fits most effectively when woven into existing lesson plans rather than added as a standalone activity. Consider which specific learning objectives each VR session will address.
Accreditation compliance
Accrediting bodies increasingly recognize VR as a valid educational tool. The Liaison Committee on Medical Education (LCME) and similar organizations have approved curricula that incorporate virtual anatomy.
Requirements vary by program and specialty, so verifying your specific accreditation standards before making significant curriculum changes is worthwhile.
Start exploring VR anatomy education today
The question isn't whether VR can teach anatomy effectively—the research has addressed that. The question is how your institution will adapt to meet the expectations of modern learners while managing practical constraints around cost, access, and scalability.
Start a free trial of the BodyMap VR anatomy platform and experience immersive anatomy learning firsthand.
FAQs about VR vs cadaver labs
How much does VR anatomy software cost compared to maintaining a cadaver program?
VR platforms typically involve subscription or licensing fees ranging from a few hundred to several thousand dollars annually per institution. Cadaver programs often cost significantly more per year when accounting for procurement, preservation, facilities, and disposal. The total cost comparison depends on student volume and existing infrastructure.
Do medical school accreditation bodies accept VR as an alternative to cadaver dissection?
Many accrediting organizations now recognize VR and virtual dissection as valid educational tools. The LCME and AOA-COCA have approved curricula incorporating virtual anatomy, though specific requirements vary by program type and specialty focus.
What VR headsets are compatible with anatomy education platforms?
Most leading platforms support Meta Quest 2, Meta Quest 3, Meta Quest Pro, and HTC Vive devices. Some also offer mixed reality experiences on newer headsets. Compatibility varies by software provider, so checking specific requirements before purchasing hardware is helpful.
Can VR anatomy training fully prepare students for surgical procedures?
VR excels at teaching spatial relationships, anatomical identification, and foundational knowledge. For procedural skills requiring tactile feedback—like suturing or tissue handling—hands-on simulation or cadaver experience remains valuable as a complement to virtual training.
Is VR anatomy training suitable for continuing medical education?
VR offers an efficient, flexible option for practicing clinicians who want to refresh anatomical knowledge or explore unfamiliar regions without traveling to a physical lab. The self-paced nature of VR learning fits well into busy clinical schedules.
Begin your VR anatomy journey today, sign up for a 7-day free trial.
Curriculum Integration Guides
Learn how to navigate the 3D model and utilize the tools to master human anatomy—all in one place.

.avif)


.avif)


.avif)